Osteoarthritis of the knee can be debilitating and reduce one’s quality of life.
Dr. Howard Luks of the Physio Network has 10 Recommendations To Thrive With Osteoarthritis of the Knee, including remaining active, managing our diet properly (hint: processed foods are a no-no), and managing/monitoring our inflammation.
This was originally posted on Dr. Howard Luks’ website, You can click here to read more blogs from him. Reference the article below to read more on Dr. Luks’ recommendations for living with OA of the knee:
Osteoarthritis of the knee is a prevalent health issue. Despite a diagnosis of arthritis of the knee, the majority of you can live an active, happy life. But you’ve heard awful phrases used to describe your Xrays– phrases like Bone on Bone, bone spurs, degeneration, wearing away, etc. Those phrases scare you. I get that!
Life does not stop after a diagnosis of arthritis. Exercise is perhaps the best medicine for your arthritis. Exercising a joint that you’ve been told is wearing out may seem counterintuitive. Exercise is essential if your goal is to avoid surgery for as long as possible. Being active will not cause your arthritis to worsen. Not all pain implies harm.
We are going to change the narrative about osteoarthritis of the knee. For the majority of you, there is hope— and a decade or more of living the life you want to lead before you need to worry about your knee osteoarthritis affecting your quality of life.

Tina is a wonderful 63-year-old nurse. She loves her work, and she’s superb at what she does. On the weekends, she was the lead singles player on her tennis team. Tina has two years remaining before she retires. Her plans have ebbed and changed over the years, but she planned on ending up somewhere warm so that she can be more active outside year-round.
Knee osteoarthritis is not a terminal diagnosis
Unfortunately, many of you have a significant misunderstanding of why osteoarthritis occurs and how to manage it. That’s not your fault. Doctors and other healthcare professionals should do a better job of describing what is happening in your knee joint. Your misconceptions about osteoarthritis often lead to self-imposed activity modifications, depression, fear, and perhaps emotional harm. Harm is part of the equation because you may not have been told that you can live an active life with an arthritic knee, and it’s not the end of the world.

Narrow joint space due to arthritis
One day Tina woke up with a swollen knee. Her knee felt stiff and achy, but the pain wasn’t severe. This followed a weekend-long tennis tournament and a long hike with her friends, so she wrote it off to over-exertion. Two weeks pass, her swelling persists.
Tina passes by an Urgent Care center on the way home, so she stopped in. Tina was told that her knee X-rays showed severe osteoarthritis. This devastated her. There was no space between the bones on the X-ray. Tina withdrew from her upcoming tennis match.
How should we discuss the causes of knee osteoarthritis?
Far too many of you are told that you wore away your cartilage. Some of you may have been told that your running caused this, or that you walked too much at work for too many years. Those theories are wrong. Osteoarthritis is often found to be less common in runners. When your healthcare providers use analogies such as a cheese grater, or sandpaper on wood, those misconceptions about the etiology or cause of your arthritis becomes your new reality.
Terms such as degeneration, aging, and wear and tear are tossed around. Words can harm. Using an inappropriate analogy can give people the wrong impression. I’ve seen this movie often… and the finale never changes.
Osteoarthritis does involve thinning or loss of the cartilage or cushioning on the ends of your bones. This is articular cartilage. This is different than the meniscus cartilage you hear about all the time.

Copyright Medical Media Group.
For the majority of you, the cartilage was not worn away because of a mechanical process. Arthritis development is a biological process. I’ll be brief here because I wrote an extensive article on osteoarthritis causation here. It turns out that our DNA, RNA, and hundreds of chemicals, protein, and hormones determine if your cartilage is going to become thinner and less resilient. Yes, this graphic below is complicated, and it should be because it’s meant to show you that this is a very complicated process.

Attribution:https://www.sciencedirect.com/science/article/pii/S1063458414012801
Tina grew very depressed. She hadn’t played tennis in nearly four weeks by the time I saw her. She stopped going to the gym, she tried to park closer at work and avoided the stairs. She was no longer going walking during her lunch break. The interesting thing was—her knee was no longer swollen, and it wasn’t hurting her. So why was she avoiding these activities?

You cannot unsee your MRI or X-ray results. Visuals can have an enormous impact on us. Combine that with a poorly articulated discussion about why osteoarthritis is present, and a very limited discussion about how to manage your new diagnosis– and real harm can occur.
Think about it… In an effort to minimize harm to her “bone on bone” knee, Tina has increased her risk of developing heart disease, stroke, dementia, and a host of other chronic diseases because she curbed many of her healthier activities.
Tina came to my office. I look forward to these conversations. This is one of those visits where you can have a dramatic impact on someone’s quality of life, all without medications and without a date for surgery. Tina and I had a long talk. We focused on why she developed osteoarthritis, and we adjusted the misconceptions she had about how to manage it. More important… we focused on how to continue to thrive and lead an active life, despite the images she cannot seem to forget.
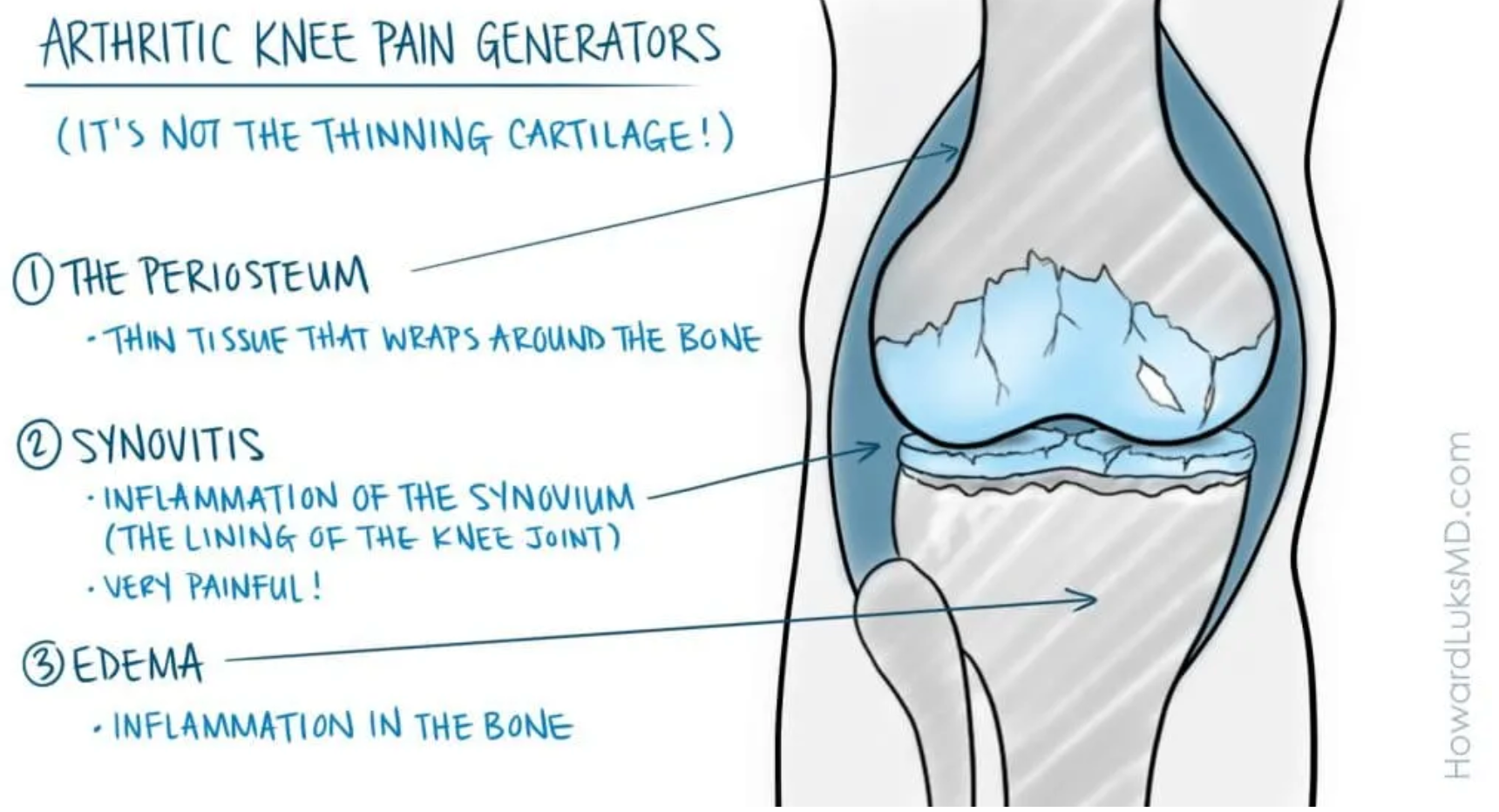
What hurts in an arthritic knee?
Believe it or not, the bone on bone arthritis of the knee may not be a “pain generator.” There are no nerve endings in the bone itself. So if two bones are rubbing together and all else is well, they won’t hurt. The cartilage in the knee also does not have nerve endings in it. So thinning cartilage will not hurt in and of itself.

There are three main contributors to the pain experienced by people with osteoarthritis of the knee. The first is the periosteum. The periosteum is a thin tissue that wraps around the bone. It supplies blood to the bone, and it does have nerve endings. Anyone who has broken a bone knows this very well. It is the tearing of the periosteum that leads to a lot of the pain.

Inflamed synovium: notice how red and “angry” it looks.
The second issue that can cause knee pain and swelling is the synovium. The synovium is the lining of the knee joint. It’s like a balloon that surrounds the bones of the knee. There are many nerve endings there. Synovitis is inflammation of that lining tissue or synovium.
Synovitis can be a very painful process. As an aside, for people with pain due to synovitis that does not respond to time, ice, heat, medications, ,etc– a relatively new procedure called a genicular artery embolization has shown significant promise at eliminating that cause of knee pain. You can read about a knee embolization procedure here.
The third contributor to pain in an arthritic knee is edema or inflammation in the bone itself. This occurs more often in women because of some degree of osteopenia or osteoporosis. That makes the bone a little weaker. So when the cartilage thins, the cushioning is also thinning. Less cushioning may cause increased stress in the bone, which can cause edema. Bone marrow edema can cause a deep, intense ache.
NOW… this is critical to understand. Not everyone with osteoarthritis will have synovitis, bone marrow edema, or pain due to the periosteum. And if you do have pain because of those issues, it will often calm down after a few weeks or months. For the majority of you, the status of your knee will return to baseline once again.
Despite all our best efforts, some of you might have severe pain that ultimately proves to be unresponsive to non-surgical measures. For you, a knee replacement may be the right alternative.

10 Ways to Thrive and Remain Active With Knee Arthritis
1. Change the narrative… you’re not wearing your knee joint out by exercising. Walking or playing tennis, as long as the pain is mild, is not going to shorten the lifespan of your knee. Quite the opposite! The stronger your legs are, the more flexible you are, the more active you are, the longer you will go before needing to consider surgery. We have some excellent reading for you to support this.
A. Why exercise improves arthritic knee pain.
B. Muscle mass, strength, and longevity
C. Why we should focus on leg strengthening
D. Does leg strengthening help prevent knee arthritis?
Common analogies like cheese being grated or sandpaper on wood just aren’t accurate. You are not wearing away your knee by walking, stretching, weight training, or exercising. If your pain level is a 3-4 or lower, you should probably keep going. Pain does not often imply that you are causing harm.

2. Treat the patient — not the Xray: This is so critical. X-rays do not tell us the whole picture. I know people with horrible looking Xrays who are running marathons. I know people with severe pain and very mild changes on an x-ray. We do not treat Xrays; we treat people.
Do not consider surgery on your knee based solely on the way your Xray looks.
Do not curtail your activities simply because of how your Xray looks.
The treatment should be geared towards your symptoms, your complaints, your exam, and your Xrays combined. Your X-rays alone are only a small part of what will contribute to my recommendations if I see you in the office.

3. Exercise: It bears repeating; exercise is not going to cause your arthritis to worsen. It may cause discomfort, especially for the first few weeks of a new exercise program– but that does not mean you are causing harm to your knee. The more flexible your knee joint is, the stronger the muscles are that support the knee joint, the better your quality of life will be. There are four pillars to an appropriate exercise program. Walking alone is not enough.
4. Aerobic exercise: Aerobic exercise implies that you are getting your heart rate up. The best aerobic exercise is the one that you enjoy doing. Some great examples of aerobic exercises are walking, jogging, riding a bicycle, using a rowing machine, treadmill, elliptical trainer, and so on.
Aerobic exercise improves your cardiovascular system, improves your metabolic health, decreases your risk of stroke, heart attacks, dementia, and other chronic diseases. Walking often helps arthritic knee feel better because it stimulates the production of your natural anti-inflammatories like IL-10. This article on my site discusses these changes in more detail.

Examples of Leg Exercises: Learn them from a professional, so your form is proper.
5. Resistance exercise: Resistance exercise implies that you are pushing or pulling something heavy. You can complete an exercise program with only your bodyweight. You do not have to spend money on a gym membership.
You will not make your arthritis worse by exercising. Of course, resistance exercise involves a small risk of injury, but that risk is lower than the risks to your overall health and well being caused by not exercising.
We covered how resistance exercise improves our health in this post, and why those exercises should be focused on your legs in this post.
6. Balance: You are catching your toes on the carpet more often, you are stumbling a bit more, and occasionally when you get up from a chair, you feel a little more wobbly. As with our muscle mass, our balancing abilities start to diminish as we age.
Our ability to balance will contribute significantly to our chance of living a longer, healthier life– free from injuries sustained as a result of falling.
Balance training also improves the sense of joint stability. Our walking becomes more confident, our fear of falling diminishes, and our risk of falling diminishes. This article that I wrote went into a lot more detail about the importance of balance training, and it provided some videos to consider doing as part of a balance training program.

7. Your diet and your metabolism. Our diet contributes significantly to the overall disease burden that many of us suffer from. Our standard American diet has led to an increase in heart disease, diabetes, fatty liver disease, dementia, and so on. Our diet and its downstream effects on our body can also cause osteoarthritis and other causes of joint pain. We covered how our diet and metabolism affects our joints in this article.
Processed foods are not our friends. It is safe to ignore the loud and angry one-sided online discussions about diets. The diet that works best for you will be one that is based on whole foods, not boxed foods. That diet will be sustainable and something that you can continue with in the long run.
The diet with the most science to support its use is the Mediterranean Diet. I have found that many people can adopt this diet with minimal difficulty.
Other diets that I have helped people adopt are whole food plant-based diets, keto diets, whole food plant and fish-based diets, and so on. The key is that we are eliminating processed carbs and processed foods as much as possible.
Have I seen people succeed with keto diets, and so on, yes. But the overall makeup of your dietary needs will be dependent on your medical history, the medicines you are taking, and a diet that you feel will be sustainable. For example, a keto diet may kill you if you are taking diabetes medications, and you are not closely monitored. But a keto diet might get you off your diabetes medications if it is appropriately supervised. So if you have any significant medical issues, please discuss your planned dietary changes with your doctor first.
One key issue is to eliminate as much added sugar as you can tolerate. Start easily. Remove all sweetened beverages. Water should be your primary drink.
Sports drinks are NOT your friend. Those added calories add up very quickly. The fructose in those drinks is a cause of liver issues such as NAFLD. Fructose will also increase your Uric Acid level. Uric acid was only thought to predispose you to gout. Now we know that your uric acid level may predict failure after certain heart procedures, it may have a role in heart disease emergence, and it can contribute to joint and tendon problems. If your uric acid level if above 6.5, you should talk with your doctor.
Next, we start to eliminate other sweets such as donuts, cookies, and so on. We start eating nuts and berries instead of packaged sweets.

Removing added sugar and processed carbohydrates (bread, rice, cereal, cookies, etc.) will also decrease the glucose burden our body needs to deal with. This can help control diabetes, reduce your risk of fatty liver, and it could decrease the level of inflammation within your body, which will increase the rate of arthritis progression and the pain you experience.
8. Inflammation: Talk about a complex topic! Inflammation is a critical variable in the causation of heart disease, liver disease, dementia, diabetes, pain, and so many other chronic disease states. Our diet and our activity levels can directly affect the levels of inflammation in our bodies. We measure the level of your inflammation with tests like:
- ESR
- hs-CRP
- Fibrinogen
and other less well known inflammatory biomarkers or mediators. Your ability to metabolize and dispose of glucose via your insulin will affect your level of inflammation. So if you are pre-diabetic, or diabetic, the level of inflammation in your body is often very high. For those of you with Type 2 diabetes, you can improve your glucose metabolism and disposal. And you should not be looking for a better pill.
Managing Type 2 diabetes is far different than implementing strategies to reduce the chance of developing diabetes. I could rattle off 100 reasons why you should take this seriously. The most important of which is that you will live a longer and healthier life. Not to be diminished is the fact that you will have less pain.
People with elevated fasting glucose (diabetes or pre-diabetes) have a higher pain response than non-diabetics. That is due to inflammation, as well as an issue with AGE’s, which we will cover in a different post one day. That means that a metabolically healthy person and a person with diabetes who have the same diagnosis will often have different levels of pain. Your nerves, your synovium, tendons, and cartilage do not appreciate the inflammatory burden of chemicals that accompany diabetes and related metabolic issues.
Have you been told you do not have diabetes because of a normal Hemoglobin A1C? Well… that is a very poor predictor of your risk of developing diabetes. You will be “insulin resistant” for years before you develop diabetes. It is essential to identify the people who will be diabetic soon. Working on your diet and metabolism at this stage will improve your lifespan, healthspan, and decrease your pain due to osteoarthritis and other causes of joint pain. This post we wrote discusses insulin resistance in more detail.
To determine your risk of developing type 2 diabetes and see if you are insulin resistant, you should ask for fasting insulin and fasting blood glucose levels. They will show that an issue exists long before your A1C rises.
9. Tai Chi: The yoga people will @ me… but if you are not used to yoga, then starting now might not be the best treatment strategy. Forcing arthritic joints into extreme positions might cause more pain. Certain yoga programs may help, but forcing yourself into certain motions may not. Tai Chi is a great way to achieve flexibility, strength, and balance training. The mindfulness component can be useful, as well.
There have been a few research articles that have shown in randomized controlled trials that Tai Chi is very useful in the management of knee pain due to osteoarthritis.

If possible, choose to be active.
We have covered lifestyle modifications and issues that affect our risk of developing osteoarthritis. We have covered topics that can help decrease the pain and disability associated with osteoarthritis. For many of you, nothing more is necessary. For those of you who still have pain despite these modifications or you want other strategies to minimize the pain while you implement those strategies, let us review a few more options.
10. Medications/Supplements/Injections: Heat or cold? I am asked this constantly. Ice will not control chronic inflammation. If ice makes your knee feel better, then use it. If it doesn’t make your knee feel better, then do not use it. I have seen people respond very well to moist heat more than I have seen people react well to ice. This is a modality used only for pain relief, so if it helps your knee feel better, then please use it.

Compression sleeves: Simple compression sleeves, without straps, hinges, etc seem to provide a number of osteoarthritis patients with pain relief. These compression sleeves must fit well, and should not be too tight. These sleeves improve your sense of stability which can improve pain and that feeling of giving way. Here is a shortlist of some good examples of knee sleeves that may work well for you.
Capsaicin: Capsaicin is an active ingredient found in many of the ointments you see on the market for managing the pain of osteoarthritis. Capsaicin is an irritant. So by applying it to your skin, the counter-irritant theory is that you may focus on the irritant and not the pain in the joint.
Capsaicin will also cause the nerves in your body to remain active because of irritation. It is believed that the constant irritation will deplete your nerves of substances that cause pain. In essence, it puts the nerves on overdrive, so they can’t send out strong pain signals back to the brain. Many people find these rubs to be useful. They can cause burns in some people, so be careful.
Topical NSAID / Oral NSAID: NSAIDs such as ibuprofen and naproxen have a role in managing the pain and swelling associated with osteoarthritis. Preferably you do not have to take them every day. People with asthma, hypertension, kidney disease, ulcers, heart disease, and people taking “blood thinners” should consider taking acetaminophen instead. NSAIDs will not stop arthritis from progressing. So you should only take it if the pain and swelling require it. NSAIDs can cause ulcers, as well as kidney disease.
Glucosamine/Chondroitin Sulphate: The research into these supplements is mixed. Most of the research shows that it doesn’t work when compared to a placebo. But what that research doesn’t tell you is that people often have a response, they feel better. So whether or not it is a placebo response or not– I’m not sure that matters. I have plenty of patients who take this regularly and insist that it helps their knee pain. These supplements will not stop arthritis from progressing, and they will not grow new cartilage.

Injections: For a long time, cortisone injections were given to people with knee osteoarthritis like water. Cortisone has harmful effects on your cartilage. Cortisone injections should not be routine and should be considered in very few situations. Occasionally someone will come into the office with a very “hot” knee. The knee is swollen and very tender. They have severe pain with motion, and these folks are not sleeping well. A cortisone injection will help calm the pain down… but we do not know how long it will last for. It may help for days or months.
Cortisone injections have a very limited role in the management of knee pain due to osteoarthritis. They are not without risk. People with diabetes will experience a significant rise in their blood sugars, and you should be prepared to manage this.
Gel, “rooster comb,” or visco injections. There is a ton of misunderstanding about these injections. They do not grow cartilage. They do not increase the space between your bones. We do not know why they appear to cause relief in some people. Many patients swear by these injections and get them every 6-12 months. Some research shows that the benefit is the same as a placebo. Other articles suggest that the benefit is more significant than a placebo. Bottom line… these injections may be an expensive placebo. But the risk of harm is low, so if you respond to them, and you understand the risks, then you and your doctor should discuss whether or not you want to try them.
Tina is back on the tennis court. She has her aches and pain, but she tolerates them just fine. She follows an exercise regiment to keep her legs strong, and she has adopted a whole-food, plant-based diet. A little bit of knowledge, a better contextual understanding, and a stable lifestyle strategy can also help many of you avoid over-treatment and self-imposed harm.

When should I have a knee replacement?
Great question !! The person in the examining room who determines when you should have a knee replacement is you. This is predominantly a quality of life procedure. Therefore only you can determine if your quality of life is affected enough that you are willing to assume the significant risks associated with joint replacement surgery. If a surgeon tells you to have knee replacement surgery simply because you have bone on bone changes on your Xrays, then you are in the wrong physicians’ office.